This report was written with the support of the Check Global COVID-19 Microgrants program and Meedan. A version of this piece, our final situation report following months of COVID-19 reporting on SyriaUntold’s Arabic site, was first published here.
By May 2020, months after COVID-19 had spread worldwide and been declared a pandemic by the World Health Organization, Syrians were doubtful of the strangely low official figures released by the government.
The virus had already spread within neighboring Iraq, Jordan, Lebanon and Turkey. But in Syria, the government had only announced 50 cases of the virus within its borders in May. Syrians were wondering to themselves and, sometimes, whispering to their family members, where are our COVID-19 cases?
Curfews were ordered in some government-controlled areas in March, amid rumors that the virus had entered the country via fighters from Iran. The measures seemed lenient, and they were often breached amid corruption by the regime, with its mafia-like structure, according to residents. Exceptions to the evening curfew were abundant in the streets. Funeral services prepared by influential people went on as usual, as the police did not dare forbid them. Soldiers moved around the country unhindered.
Khuloud Saba, a public health researcher at the University of Edinburgh who focuses on Syria’s medical system, tells SyriaUntold that government handling of the pandemic has been failing due to “information blackout, data loss and lying” on the part of Damascus.
She adds that in much of Syria, “there is no system to collect and share information, which is key to fighting the virus, tracing the epicenters and mapping the virus spread. The guidelines to fight pandemics require steps to diagnose, test, trace and contain them. The government here is only good at denial.”
Due to quarantine measures adopted in early spring, which kept individuals away from their families and homes, and with authorities’ requests for residents to report any suspected, symptomatic COVID-19 cases, people who caught the virus were stigmatized. Those who became sick feared revealing that they were infected. As a result, it became more difficult to determine how widely COVID-19 had spread in Syria.
According to Saba, Syria and other countries in the region were similar in how they handled the pandemic. But Syria stood out because of data “blind spots.” Movement between military checkpoints, cities and from foreign countries went unsupervised. Suspension of classes in schools and universities, the significant decrease in the activity of markets and restaurants and the legal ban on movement between cities were introduced early on, and this was enough to protect citizens of those areas from a more massive spread of the pandemic, despite the numerous breaches.
Still, the virus spread.
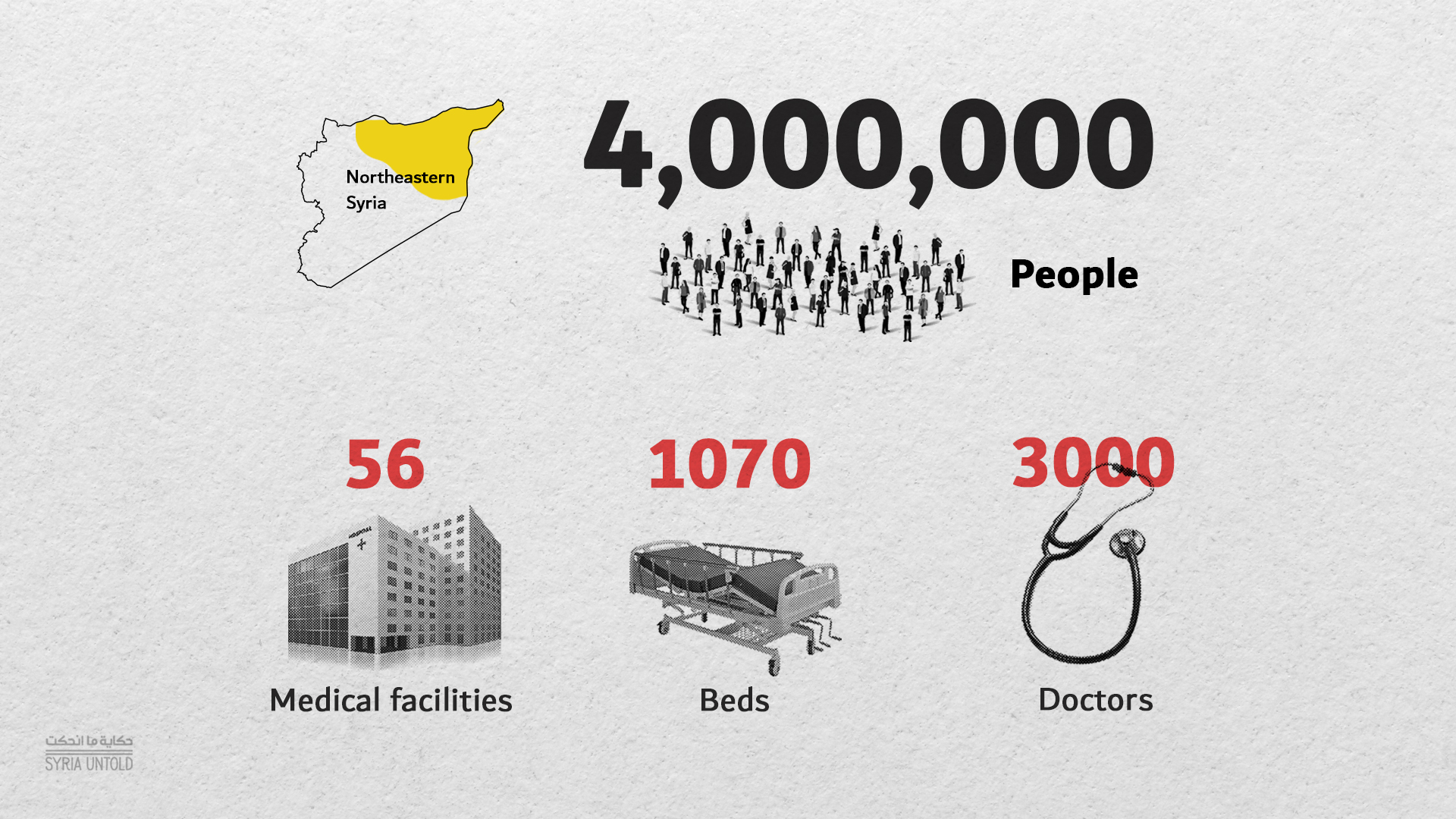
Northeastern Syria
Syria’s northeast, which is largely governed by the majority Kurdish Self-Administration, was not spared a reckless public health strategy. The regime refused to coordinate with local health management institutions, and travellers continued to enter Qamishli from the Damascus airport without quarantining, not to mention the US and Russian forces whose movement there was unmonitored, even as infections may have spread among soldiers.
The World Health Organization (WHO) office in Damascus apparently did not even bother to notify local Self-Administration authorities of a confirmed COVID-19 case in April after the result of the PCR test done in Damascus came back positive.
The Self-Administration released a statement afterwards blaming the WHO for the pandemic outbreak in its areas. Meanwhile, authorities in the northeast managed to convince residents to adhere to the remaining general prevention measures to a reasonable extent. The spread, for a time, remained at minimum levels in an area with among the weakest health infrastructures in Syria.
Whereas government and Russian airstrikes directly bombed medical facilities in Syria’s opposition-held northwest, hospitals and other facilities in the northeast have suffered decades of systemic neglect from successive Baathist regimes. According to available figures, there are most likely 56 hospitals and around 3,000 doctors in the area, with a population of four million people.
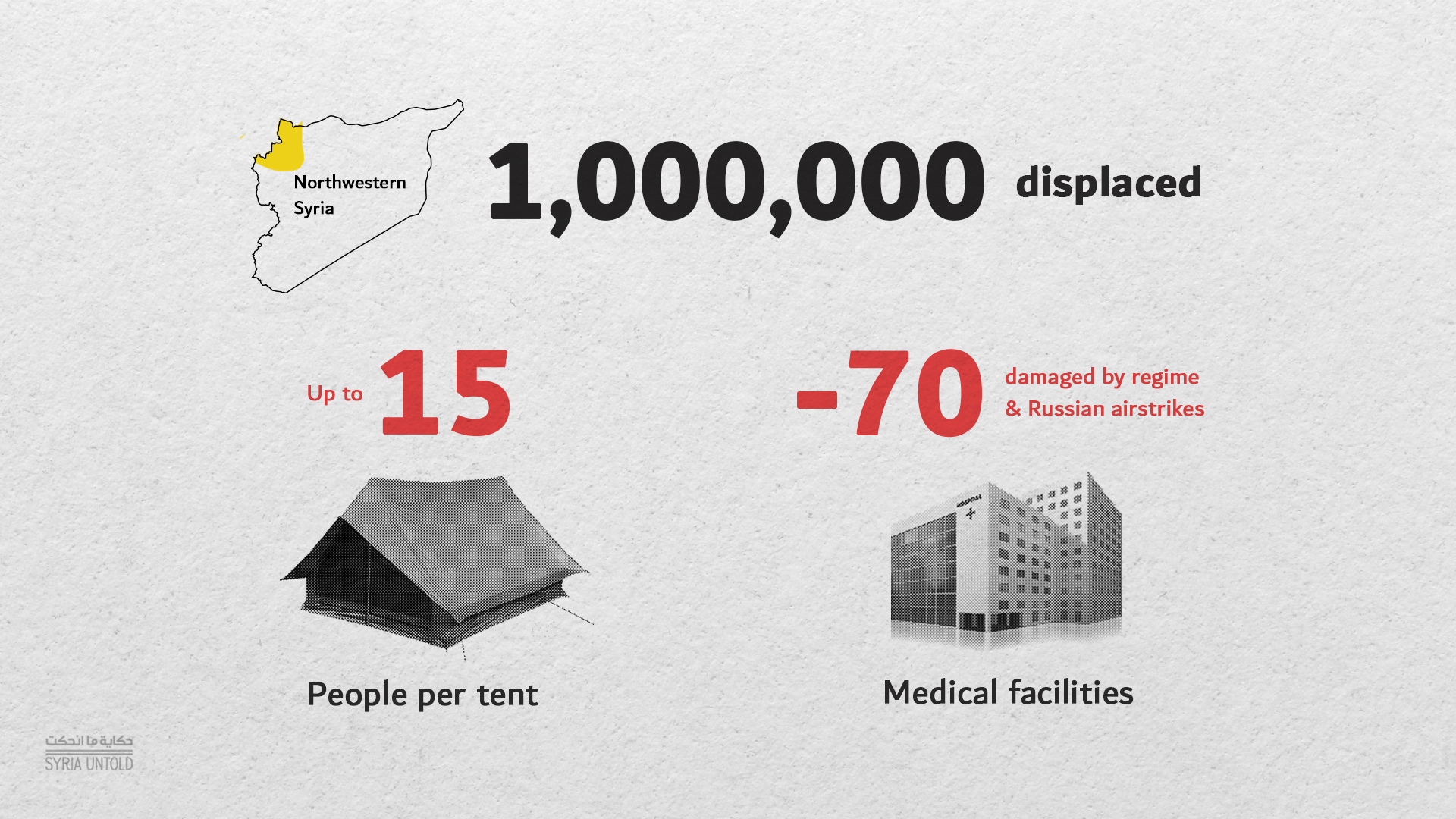
Idlib and its surroundings
In the northwest, crossings with the regime-controlled areas were closed, as they were believed to be potential sources of the virus’ spread. However, reduced trade movement continued across the border with Turkey.
Those working in the medical sector and in civil organizations were fearful, aware that many medical facilities had been either damaged or completely destroyed by Syrian and Russian bombing, particularly over the past year. In addition, many residents complained over social media that WHO recommendations for social distancing and sanitizing were “elitist” in an area where more than one million people are living in crowded, poorly served displacement camps with the bare minimum of water and health standards. In some tents, up to 15 people lived crammed together.
Still, the area remained safe from the pandemic for months during spring, given the lockdown, restrictions on movement between cities and towns and the suspension of schooling. Regarding medical coordination with regime-controlled areas, the director of one of the Idlib hospitals told SyriaUntold on condition of anonymity that some health workers in regime areas were more cooperative as per their own initiative, regardless of instructions.
“They clearly felt the situation was serious this time, after having experienced previous political and security impediments to coordination, including the polio vaccination campaign in 2014,” the hospital director said.
Syrian government: lifting the lockdown
By the end of May, the Syrian government decided to lift the lockdown completely and resume normal life without any significant precautions, except for imposing masks on residents visiting public institutions, and checking the temperatures of university students when they were on campus.
But these measures could oftentimes be circumvented with bribery and corruption, as SyriaUntold reported in September.
The virus had reached every quarter in Damascus by July. Those questions whispered between family members had received their answer, and Syrian people began preparing to stave off COVID-19 in the same way they confronted all previous infrastructure collapses: by making do without.
No preparation
With the low number of ventilators, quarantine beds and the intensive care units, Syria was clearly unprepared to care for people infected with COVID-19. Damascus, which has the country’s strongest service infrastructure, is home to only 15 government hospitals, including specialty facilities such as an eye hospital and a hospital for mental illnesses, to cater to millions of people.
Hopes of any improvement seemed bleak, given bureaucratic corruption in official response measures. Medical staff repeatedly wondered about the fate of aid supplies that the government received from its strategic allies and WHO, amid their work in dangerous conditions where the minimum protective equipment was lacking. According to the declared death rate, more than 60 doctors died by late August as a result of treating patients infected with the virus.
Protective gear, tests and their sale licenses were monopolized, and travelers had to undergo PCR tests costing university graduates the equivalent of four months of salaries. Patients in need of ventilators were not admitted to government hospitals unless they paid a substantial bribe. Out of 110 ventilators in Damascus city, only one-quarter were reportedly available in government hospitals, and there was no intention to increase this number, even if the funds were available. The director of Damascus’ Ibn al-Nafis hospital, a state-run facility, told the pro-government Thawra newspaper in March that ventilators were not the priority of hospitals, which preferred to invest in buying other equipment.
Khuloud Saba, the public health researcher, notes that “the number of intensive care beds and ventilators is not the issue. Numbers out of context are not useful, and they might be used to give media credibility to one party or the other. In the presence of a pandemic, a general system for all cases, whether critical or otherwise, must be in place.”
She adds: “Pandemics are not fought individually, but collectively. A failed state cannot provide social protection to anyone.”
And ironically, the extreme isolation of some long neglected areas of Syria, including many rural regions, may have protected those places from the scale of infection seen in the cities, Saba says.
It never rains, it pours
The COVID-19 outbreak coincided with successive economic crises: from the banking and governmental shortfalls in neighboring Lebanon and the sharp depreciation of the Lebanese Lira, to the financial scandals outed in the media by Bashar al-Assad’s maternal cousin, business tycoon Rami Makhlouf, and his disputes with his Assad’s wife Asmaa, to the Caesar Act sanctions and the accumulated repercussions of the years of war. All these elements together contributed to the fastest plunge of the Syrian Pound (SYP) since 2011, despite comparative calm on military fronts.
Pandemics are not fought individually, but collectively. A failed state cannot provide social protection to anyone. -Khuloud Saba, public health researcher
The medical sectors bore the brunt once again. Pharmacies went on a near-total strike in springtime because pharmaceutical industries would not make purchases at the official exchange rate, which the government wanted to impose on foreign trade transactions. They called for raising the price of medication in line with the increasing production cost in SYP. The exchange rate difference fluctuated between 435 and 3,600 SYP against the dollar at the time.
Ultimately, the pharmaceutical industries were permitted in June to increase the prices of some medications, such as paracetamol, from 50 to 850 SYP. Still, employees’ salaries were not raised, and the most qualified employees, like engineers, doctors and university professors earned up to the equivalent of $30 per month, compared to $600 a decade ago.
For young Idlib doctors who treated war wounds, COVID an invisible new threat
02 October 2020
Economic observers have not yet managed to calculate the full financial damage of the pandemic on Syria, nor have they isolated the pandemic’s damages from the damages resulting from other economic difficulties. So far, the losses stemming from the closure of economic facilities during the lockdown are mere speculations and have been estimated at $1 billion per month.
According to Joseph Daher, a political science scholar at the University of Lausanne and the European University Institute in Florence, COVID-19 has exacerbated pre-existing economic problems in Syria, but it did not create them. The fluctuation of the currency started with the revolution, and the latest plunge technically began at the end of 2019, when the dollar was equivalent to less than 600 SYP and reached 1200 SYP in January.
“COVID-19 has affected money transfers specifically, as they were hit by the deteriorating global economy, not just the weak economic performance at home,” Daher tells SyriaUntold. “And, the global economy will not have a fast recovery in the near future. According to the latest estimates of the International Monetary Fund in 2016, annual transfers were estimated at $2 billion ($4 million per day), constituting around 10 percent of gross domestic product.” Citing an economist in Damascus, Daher says transfers may have dropped to half their previous rate, though it is unclear how exactly that estimate was reached.
The border closures during lockdown only added to the losses, as many Syrians relied on cash entering with travelers due to their mistrust in official money exchange and transfer offices. The gap widened between the government-imposed official exchange rate and the actual market rate outside Syria.
Role of civil society
Civil society was preoccupied with making do without, as usual. Facebook groups were created to exchange medications, to avoid throwing away any drugs a sick person might need and could not find in pharmacies. Charities and newly created volunteer groups, such as Akmha, which is involved in public hygiene campaigns, engaged in individual initiatives to deliver oxygen canisters to the doorsteps of patients so that they would not need to leave their houses.
Susan, a former aid worker in Damascus who requested a pseudonym for safety, tells SyriaUntold that “people are now contacting Akmha instead of ambulances.” She describes a lack of trust in official medical services and, instead, a large scale reliance on civil society initiatives as a more effective alternative.
“They often provide free, fast delivery of oxygen canisters to houses. But, of course, the demand is higher than what they can cater to. There is only so much they can do,” she says.
At the peak of the outbreak during July and August, many Syrians decided they preferred to be treated at home, especially after the official declaration of a large number of deaths among health workers who were in contact with infected patients, and the concealment of the remaining deaths.
Doctors publicly demanded on social media that authorities shut down and sterilize Al-Mouwasat Hospital in Damascus, after it became a hotspot avoided by healthy and sick people alike.
There has to be a unified medical authority that standardizes general symptoms in the whole country before claiming that COVID-19 in Syria is different from COVID-19 in Iraq or other countries. -Khuloud Saba
Hala, a high school teacher in Damascus, says that she and her university-age daughter both caught COVID-19 in July. “Our daily routine was home, clinic, pharmacy and back,” she says, using a pseudonym to protect her safety. “We had our masks on, and we took our medication. We did not go to the hospital or come near to it. We stayed at home for three weeks, and we are fine. It’s all the same.”
In other areas, delaying the peak of the virus helped improve infrastructure and preparedness, even though the situation was still less than ideal. PCR tests arrived to the northeast from Iraqi Kurdistan in late April, before the ones the WHO had promised to deliver to Self-Administration authorities.
Health organizations were able to implement some sterilization and awareness measures across areas of Syria that are outside government control, and the market was able to secure the demand for masks and sterilization materials, after their prices soared at the beginning of the lockdown. Quarantine centers were rehabilitated, hospitals were expanded and more ventilators were imported. The number of available ventilators in free treatment centers in areas outside the government control exceeded that in state-run hospitals within government-held areas. The number of ventilators in the northeast was estimated by doctors at more than 62, and in the northwest, it was close to 100, while most ventilators in government areas were found in private hospitals with ridiculously high prices, as per the new exchange rates. The outbreak of the epidemic in the northern regions remained much less than the peaks in Damascus, Aleppo and the coast, even if the figures released by official authorities in those regions were multiplied tenfold.
An effective step, and yet
For northwestern Syria, closing crossings with government-controlled areas was an effective step. But the first infection announced in the northwest, in July, entered from Turkey, followed by two infected women who were smuggled into Sarmin, a town in rural Idlib, from Damascus. The cases prompted local authorities to impose a short curfew on Sarmin.
Trust in the official measures and the health sector varied from one area to another.
COVID-19 on the Syrian coast
28 March 2020
Watching the Caesar Act unfold, from the hometown of the Assads
01 July 2020
While residents were oftentimes certain of institutional corruption in government-held areas, opinions differed in the northeast and northwest, where some people doubted the capacities of the lagging health sector due to systemic bombing. Others were suspicious about the seriousness of implementing precautionary measures, especially those fearing unemployment and poverty more than they feared the virus.
It is noteworthy that the section of the population in government-controlled Syria that has the most access to media is usually more vocal about its doubts and shares news more widely. Still, the government’s official statistics of COVID-19 infections and deaths provoked unparalleled mockery in areas outside its control, as residents there have comparatively more trust in the transparency of locally declared infection numbers.
Still, according to Saba, “all areas had one thing in common—people did not resort to the health sector when the problem started. Everybody knows that even if this sector was capable of offering its services, it has zero capacity to limit the virus spread.”
She adds: “Everybody agreed on the need to isolate patients, even in the absence of a social support system.”
For Saba, this absence was both hurtful and costly.
“If it weren’t for social solidarity and home care within the family, the deaths would have been much higher. COVID-19 patients need a lot of care that consumes huge medical resources in hospitals. Syrian women did this task. Some of them were infected and paid the price withtheir own health, while others were young and their bodies resisted. The bare minimum is to provide information to the families of patients and first-line healthcare nurses, midwives and others. The government just lied and fed them the wrong information.” .
Nature and mutations of the virus: a debatable matter
Across Syria, talk of “the mutating nature” of the virus was rampant over the summer. Health workers and infected residents, mainly in Damascus, tell SyriaUntold that they believe worst and most common symptoms were related to the digestive, rather than respiratory system. This led a decrease in demand for ventilators and oxygen tubes relative to the number of infections. Consequently, the number of fatalities dropped because most people were able to take precautions and treat themselves at home. Respiratory symptoms became less serious. Nevertheless, the conditions of people with acute respiratory problems deteriorated quickly and were sometimes fatal in the absence of ventilators.
Kinda, a doctor in Aleppo speaking under a pseudonym, recalls the condition of one of her acquaintances.
“He was in his late 60s, and he was perfectly fine during the day on a trip to Mashta al-Helou. In the evening, he began coughing and his temperature rose. The next day, he arrived in Aleppo and searched the hospitals, but none had ventilators. His body could not take it, and he died overnight. He had [pre-existing] bronchitis. There is nothing you can do.”
Many medical rumors circulated among doctors. Apparently, some were convinced that the difference in symptoms stemmed from various types of the virus. Some even said that becoming infected with one type does not make a patient immune to the other two types, amid an international struggle to discover the effectiveness of antibodies that the recovering patients produce.
“It is really tragic,” Saba says. “The elite here give wrong information, and nobody holds them accountable. The problem is not the internet rumors and lack of awareness among people, like in other countries. We cannot blame people. Each country has its own social habits to differentiate between the common cold and the influenza, for instance. COVID-19 isn’t a virus with standard symptoms, as they vary depending on age, health condition and other factors. For that reason, we cannot rely on comparing symptoms among citizens or even with workers in the health sector. There has to be a unified medical authority that standardizes general symptoms in the whole country before claiming that COVID-19 in Syria is different from COVID-19 in Iraq or other countries.”
A drop in cases?
At the end of August, healthcare workers in Damascus began talking about a clear decline in the number of infections, and they were hopeful about flattening the curve.
Hussam, a head and neck surgeon, said in early September: “An average of six to 10 infected patients would visit me daily in July, compared to one patient every two to three days now.”
Civil society organizations providing medical aid also announced a drop in the daily demand for their services during this same period.
According to a recent Reuters report, one of the directors of an international NGO in Syria noted that the daily fatalities have dropped from their peak in July and August, from 120 to 60 deaths per day in September.
However, the government continues to take social distancing lightly. The Ministry of Education insisted on reopening schools as usual, despite increasing complaints due to the lack of measures to reduce crowded classes, and despite hospital workers noting a slight increase in infections among children.
Since early September, official numbers have increased once again, although some people claimed that this was because of increased testing. Meanwhile, the government continues to hide information and has not announced the lab capacities for daily testing.
Politicizing the pandemic
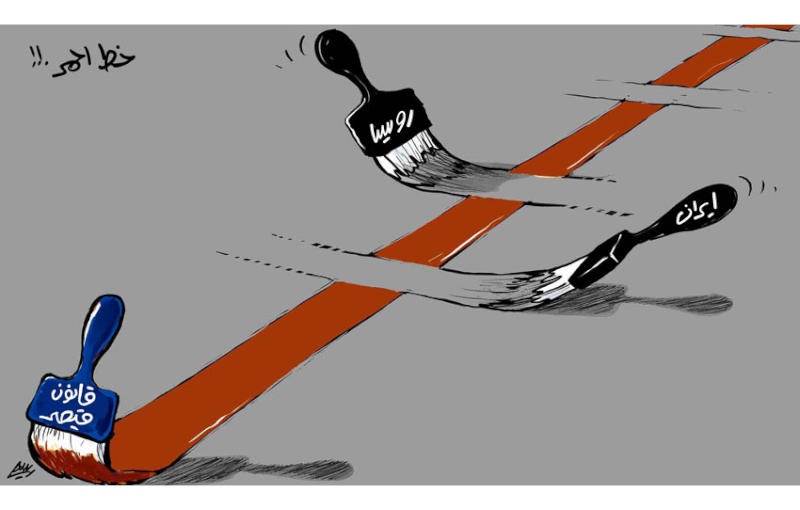
Earlier this year, Russia insisted on ending the mandate of a border crossing used by the UN to deliver international aid to the opposition-held northwest. The Bab al-Hawa crossing, between Idlib and Turkey, was the only one left for aid to pass through, and reaching the targeted beneficiaries in areas outside the control of the regime in Damascus was a struggle in itself.
In the northeast, the Self-Administration closed the borders again for travelers after infections began to rise slightly at the beginning of summer. But, wedding ceremonies and rituals in places of worship resumed in September, which led to an increase in objections from the residents left stranded outside the region due to the closure of the crossings. A decision was issued to open the crossings to them until the end of the month. The official number of infections in the region exceeded 2,300 and about 80 deaths were recorded as of mid-October.
In the northwest, cases rose significantly since early September. On one day in mid-September, positive results were found in more than a quarter of the tests analyzed. The total number of deaths from COVID-19 until then had not exceeded four in an area of about 4 million people, though by mid-October there were 14 deaths. Positive cases were recorded in 18 camps, accounting for 10 percent of the PCR tests conducted.
Economic collapse and the shocking devaluation of the currency over the past year remain the biggest problem for Syrians across the country. Fear of poverty and hunger prevailed over the ability to adhere to social distancing and quarantine measures, and the reduction of food rations distributed by the World Food Programme and the recent fires on the coast only made things worse.
In the midst of all this, the rise in cases of domestic and gender violence and killing, especially during the lockdown in spring, has gone unnoticed, as such issues have not been prioritized in recent years.
Meanwhile, workers documenting the humanitarian conditions in prisons and detention centers in all regions reported that political detention centers throughout the country are not respecting the minimum precautionary measures to prevent the spread of the virus among detainees, who are already incarcerated in poor sanitary conditions. Nobody has been able to document the scope of the pandemic spread in those prisons, where even those fighting and documenting the pandemic are not allowed access.